Multidisciplinary care for opioid dose reduction in patients with chronic non-cancer pain: A systematic realist review
Multidisciplinary care for opioid dose reduction in patients with chronic non-cancer pain: A systematic realist review
Citation
Sud A, Armas A, Cunningham H, Tracy S, Foat K, Persaud N, Hosseiny F, Hyland S, Lowe L, Zlahtic E, Murti R, Derue H, Birnbaum I, Bonin K, Upshur R, Nelson MLA. Multidisciplinary care for opioid dose reduction in patients with chronic non-cancer pain: A systematic realist review. PLoS One. 2020 Jul 27;15(7):e0236419. doi: 10.1371/journal.pone.0236419. PMID: 32716982; PMCID: PMC7384622.
Abstract
Context
Opioid related deaths are at epidemic levels in many developed nations globally. Concerns about the contribution of prescribed opioids, and particularly high-dose opioids, continue to mount as do initiatives to reduce prescribing. Evidence around opioid tapering, which can be challenging and potentially hazardous, is not well developed. A recent national guideline has recognized this and recommended referral to multidisciplinary care for challenging cases of opioid tapering. However, multidisciplinary care for opioid tapering is not well understood or defined.
Objective
Identify the existing literature on any multidisciplinary care programs that evaluate impact on opioid use, synthesize how these programs work and clarify whom they benefit.
Study design
Systematic rapid realist review.
Dataset
Bibliographic databases (MEDLINE, EMBASE, CINAHL, PsycINFO, Cochrane Library), grey literature, reference hand search and formal expert consultation.
Results
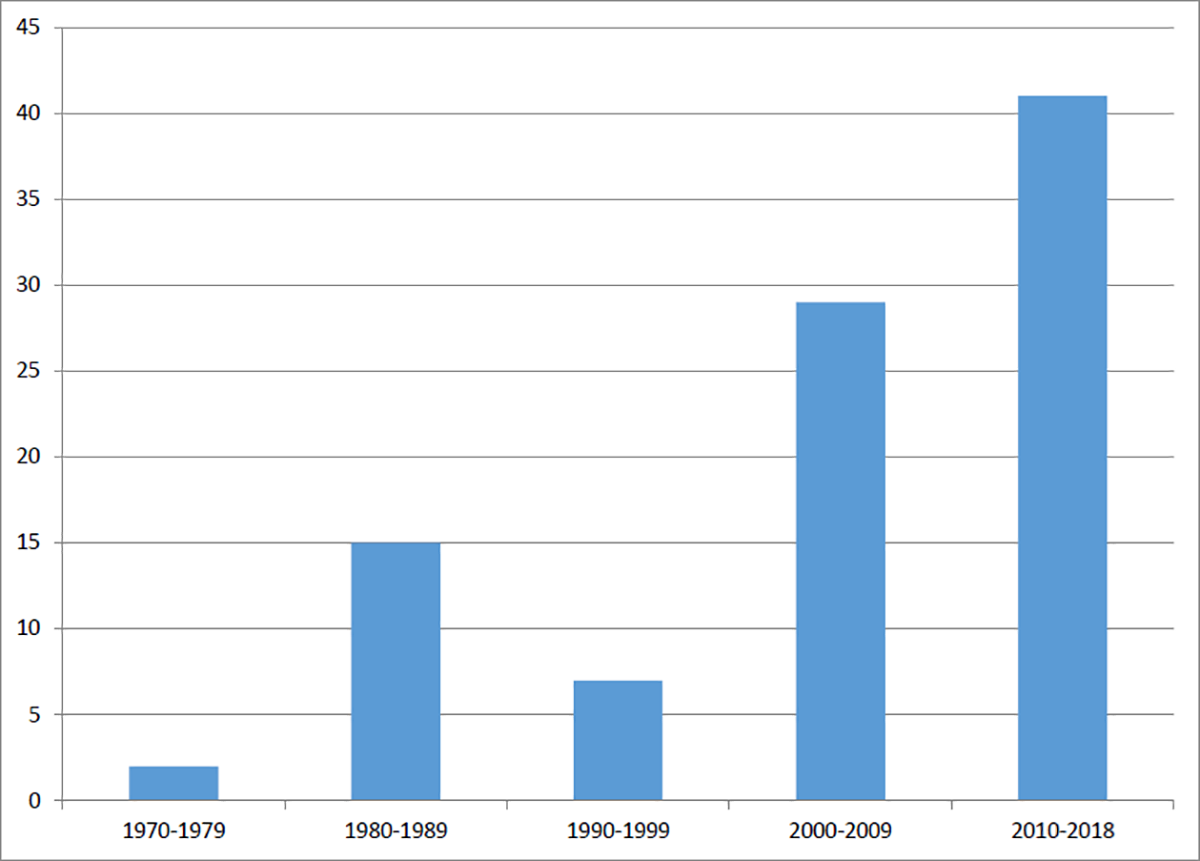
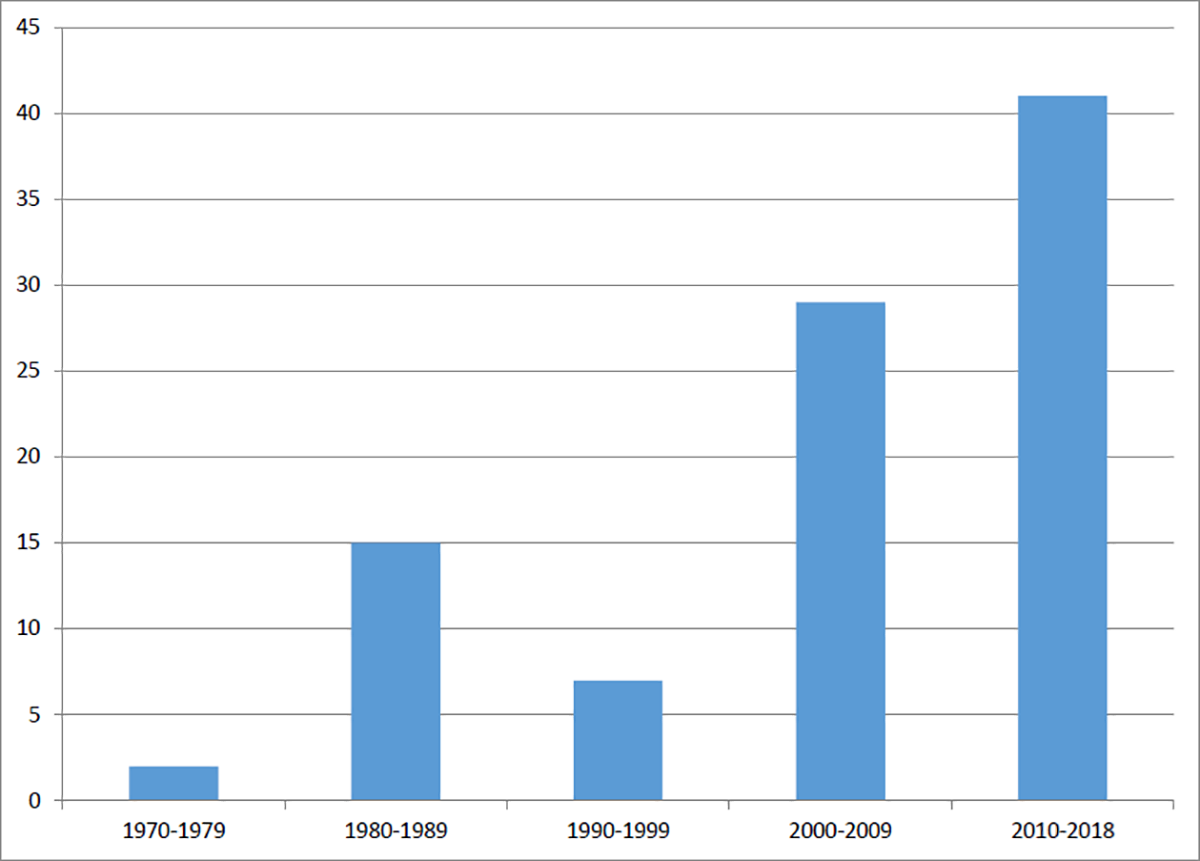
95 studies were identified. 75% of the programs were from the United States and the majority (n = 62) were published after 2000. A minority (n = 23) of programs reported on >12 month opioid use outcomes. There were three necessary but insufficient mechanisms common to all programs: pain relief, behavior change and active medication management. Programs that did not include a combination of all three mechanisms did not result in opioid dose reductions. A concerning 20–40% of subjects resumed opioid use within one year of program completion.
Conclusions
Providing alternative analgesia is insufficient for reducing opioid doses. Even high quality primary care multidisciplinary care programs do not reduce prescribed opioid use unless there is active medication management accomplished by changing the primary opioid prescriber. Rates of return to use of opioids from these programs are very concerning in the current context of a highly potent and lethal street drug supply. This contextual factor may be powerful enough to undermine the modest benefits of opioid dose reduction via multidisciplinary care.
Funding
Link